Eczema, a common and often stubborn skin condition, can significantly impact daily comfort and confidence. Recently, interest has grown around ivermectin, a medication known for treating conditions like rosacea and scabies, as a potential option for easing eczema symptoms. While ivermectin’s anti-inflammatory properties show promise, it’s important to know that current evidence does not confirm it improves the skin barrier-the core issue in eczema. If you’re exploring new ways to manage flare-ups or reduce inflammation, understanding ivermectin’s role might offer valuable insights. This article delves into what science says about ivermectin for eczema, helping you make informed choices alongside your healthcare provider.
Ivermectin: A New Hope for Eczema Sufferers
Eczema, known for its persistent itching and inflamed skin, can prove deeply frustrating for those affected. Emerging as a potential ally, ivermectin has sparked interest due to its unique approach in targeting underlying skin issues rather than just symptoms. While primarily recognized for its antiparasitic properties, ivermectin also exhibits anti-inflammatory effects that could help calm irritated skin and reduce flare-ups common in eczema sufferers.
Unlike traditional eczema treatments that often focus on hydrating the skin or suppressing immune responses, ivermectin works by addressing microscopic skin mites and bacteria that may exacerbate inflammation. These tiny triggers can worsen itching and redness for some individuals, and ivermectin’s action on the nervous systems of these mites renders them inactive, potentially easing the skin burden. This dual impact-both targeting pests and soothing inflammation-offers a fresh avenue for managing eczema symptoms beyond standard moisturizers and corticosteroids.
- Improved symptom relief: Users report reduced itching and redness after topical ivermectin application.
- Potential reduction in flare frequency: By controlling inflammatory triggers, skin may experience fewer flare-ups.
- Complementary use with other treatments: Ivermectin can be integrated cautiously alongside existing regimens under medical guidance.
It’s important to underscore that while early observations are promising, ivermectin is not a guaranteed cure for eczema and does not replace conventional treatment plans. Consulting a dermatologist before starting ivermectin ensures appropriate use tailored to individual skin conditions. This innovative option encourages hope but remains part of a broader strategy for managing eczema with careful oversight and informed decision-making.
Understanding Eczema: Causes and Symptoms
Eczema affects millions worldwide, yet its exact roots can be complex and varied. At its core, eczema is a condition where the skin’s natural barrier weakens, making it prone to dryness, irritation, and inflammation. This breakdown often triggers an overactive immune response, leading to persistent itching and redness. For many, eczema flares unpredictably, influenced by environmental, genetic, and lifestyle factors.
Key Causes Behind Eczema
Understanding eczema means recognizing it as more than just dry or irritated skin. Genetics play a significant role-if eczema runs in your family, you may have a higher chance of developing it. Environmental triggers, such as allergies to pollen, dust mites, or pet dander, commonly provoke flare-ups. Additionally, irritants like harsh soaps, detergents, or certain fabrics can worsen symptoms by further compromising the skin barrier. Stress and weather changes, particularly cold or dry air, also contribute to flare frequency.
Recognizing Symptoms and Patterns
Symptoms of eczema often begin with intense itching, which worsens with scratching and can lead to skin thickening or cracking over time. Areas like the hands, behind the knees, and around the eyes are frequently affected but eczema can appear anywhere on the body. The skin may display redness, swelling, scaling, or oozing during severe bouts. Importantly, eczema manifests differently from person to person and may change throughout life stages, evolving from childhood into adulthood.
- Itching: Often the most distressing symptom, driving discomfort and skin damage.
- Inflammation: Redness and swelling mark active eczema patches.
- Dryness: Skin often loses moisture, feeling rough or cracked.
- Secondary Issues: Broken skin invites infections, requiring prompt care.
Recognizing these symptoms early and understanding what triggers or soothes your eczema empowers better control. While ivermectin’s emerging role targets some underlying factors like skin microbes, managing eczema requires a holistic approach including gentle skin care, trigger avoidance, and professional medical advice.
Consulting a healthcare provider remains essential to tailor treatments and rule out other skin conditions that mimic eczema. Knowledge of your unique eczema pattern can transform frustration into proactive self-care and informed treatment decisions.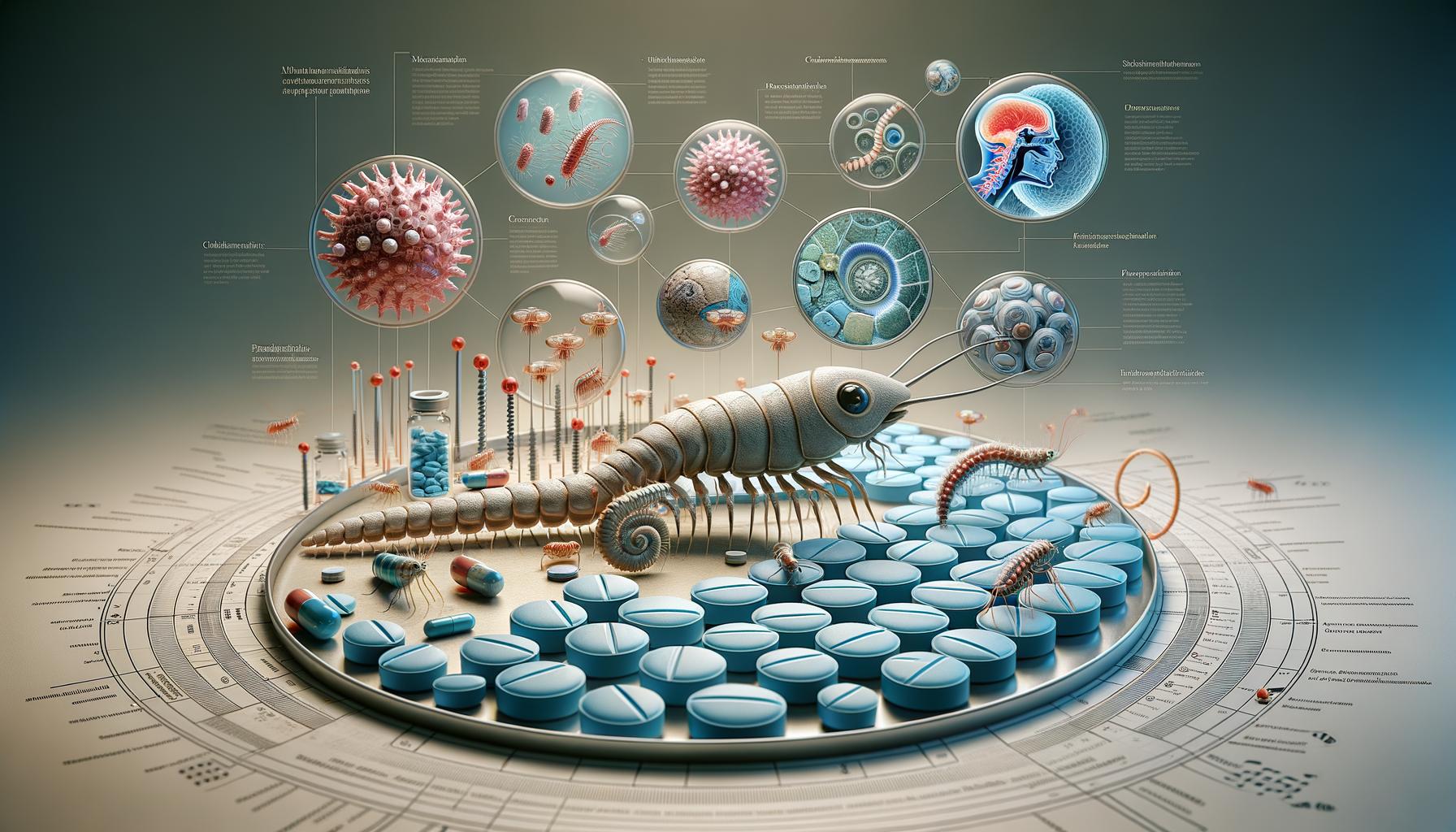
How Ivermectin Works: Mechanism of Action
Ivermectin’s potential in skin conditions arises from its multifaceted action, though its role specifically in eczema remains under scientific scrutiny. Unlike traditional eczema treatments that mainly reduce inflammation or moisturize, ivermectin targets microscopic organisms living on the skin and influences certain immune pathways, which might contribute to flare-ups in some individuals.
At its core, ivermectin is an antiparasitic agent. It works by binding to specific chloride channels in the nerves and muscles of tiny organisms such as mites or parasites, causing paralysis and death of these invaders. This is especially relevant in cases where skin conditions overlap with infestations, like scabies, which can worsen or mimic eczema symptoms. By eliminating these mites, ivermectin indirectly helps reduce skin irritation and inflammation caused by their presence. However, it’s important to note that current evidence does not confirm that ivermectin directly repairs the skin barrier defects seen in eczema [[1]](https://www.instagram.com/reel/DJ4WIF_Jb1e/?hl=en).
Beyond its antiparasitic effects, ivermectin exhibits anti-inflammatory properties. It can modulate the immune response by reducing the production of certain inflammatory molecules that drive redness and itching. This immune-modulating effect can help calm overactive immune cells in the skin, which are central players in eczema pathology. While this offers a compelling rationale for its use, the exact mechanisms and clinical benefits in eczema remain areas of ongoing research and are not fully established [[2]](https://www.jaad.org/article/S0190-9622(16)31009-X/fulltext).
Practical Considerations for Patients
- Not a primary treatment: Ivermectin should not replace standard eczema therapies such as moisturizers, corticosteroids, or calcineurin inhibitors unless specifically advised by a dermatologist.
- Potential role in complicated cases: In patients with eczema complicated by skin infections or mite infestations, ivermectin may provide direct benefits by addressing these factors.
- Consultation is key: Because its effects on eczema are not fully understood, professional guidance ensures appropriate use and integration with other treatments.
Understanding how ivermectin functions provides insight into why it might help some eczema sufferers but also why it is not a universal solution. It acts more as an adjunct therapy, with benefits tied to reducing skin microbes and dampening inflammation rather than repairing the underlying skin barrier. As research continues, clearer guidelines will emerge to help patients and clinicians make informed, safe choices. Until then, maintaining open communication with your healthcare provider remains essential.
Research Insights: Clinical Trials on Ivermectin for Eczema
Clinical investigations into ivermectin as a treatment for eczema are still in the early stages, reflecting both cautious optimism and the need for more robust data. While ivermectin’s antiparasitic and anti-inflammatory properties suggest potential benefits, existing clinical trials primarily focus on related skin conditions such as scabies and rosacea, which share inflammatory components with eczema. This indirect evidence provides a foundation but not definitive proof for its role in eczema management.
One key insight from these trials is ivermectin’s effectiveness in reducing skin mites and modulating inflammatory responses, which may alleviate symptoms in patients whose eczema is complicated by infestations or secondary infections. For instance, studies demonstrating the efficacy of oral ivermectin in scabies treatment-at doses around 400 μg/kg-highlight its ability to break cycles of skin irritation caused by mites [[1]](https://www.actasdermo.org/en-treatment-human-scabies-with-oral-articulo-resumen-S1578219017302524). Similarly, topical ivermectin has shown promise in controlling inflammation in rosacea by targeting skin mites and calming immune overactivity [[2]](https://curology.com/blog/how-ivermectin-is-used-in-skincare/). These findings hint at mechanisms that could be relevant to some eczema patients, especially those with stubborn inflammation or overlapping mite colonization.
However, conclusive randomized controlled trials (RCTs) specifically designed to evaluate ivermectin’s efficacy and safety in atopic dermatitis or other eczema types remain sparse. Some smaller pilot studies and case reports suggest symptomatic improvement, mainly where secondary microbial factors play a role, but these are not yet sufficient to change clinical guidelines. Researchers emphasize that ivermectin should not replace established eczema treatments like moisturizers, corticosteroids, or calcineurin inhibitors until more rigorous data confirm its benefits and optimal use parameters.
What This Means for Patients
- Adjunct potential: Ivermectin may serve as an add-on therapy for individuals with eczema complicated by parasites or persistent inflammation unresponsive to standard treatments.
- Ongoing studies: Stay informed about emerging clinical trials, as evolving evidence may clarify which subgroups benefit the most from ivermectin.
- Professional guidance: Always consult a dermatologist before considering ivermectin; they can help weigh current evidence against your personal condition and recommend appropriate treatment strategies.
In short, while ivermectin’s therapeutic possibilities for eczema are promising, the current research landscape calls for cautious interpretation. Ongoing and future clinical trials will be crucial to defining its precise place in eczema care and unlocking its full potential without compromising safety or efficacy.
Comparative Effectiveness: Ivermectin vs. Traditional Treatments
Eczema treatments have long centered on calming inflammation and repairing the skin barrier, using approaches like moisturizers, topical steroids, and immunomodulators. Ivermectin introduces a new dimension because it targets specific inflammatory pathways and microbial factors, including skin mites, that are often overlooked in standard regimens. However, unlike proven eczema medications, ivermectin’s role is still being defined, making a balanced comparison essential for informed decisions.
Traditional therapies such as corticosteroids and calcineurin inhibitors are well-established for reducing immune overactivity and swelling in eczema. They work broadly on immune cells to decrease redness and itching but do not directly address secondary triggers like mite infestations or microbial imbalances. Ivermectin’s anti-parasitic and anti-inflammatory effects may complement existing treatments, especially in patients with stubborn symptoms linked to these factors. This dual action is an intriguing advantage but one mainly supported by evidence from related skin conditions like rosacea and scabies rather than definitive eczema trials [[2]](https://www.jaad.org/article/S0190-9622(16)31009-X/fulltext).
- Effectiveness: Traditional treatments have robust data backing their ability to control eczema flares over time, whereas ivermectin’s efficacy is still emerging and primarily studied in small pilot cases or secondary contexts.
- Safety profile: Corticosteroids can cause skin thinning and other side effects with prolonged use. Ivermectin tends to have a favorable safety record in approved uses, yet long-term safety in eczema is not fully established.
- Mode of use: Topical ivermectin cream is usually applied once daily, which can be convenient compared to some multi-step steroid regimens; however, frequency and duration for eczema require further clarification.
| Aspect | Traditional Eczema Treatments | Ivermectin |
|---|---|---|
| Primary Action | Suppress immune response, repair skin barrier | Anti-parasitic, anti-inflammatory, targets mites |
| Evidence Base | Strong, supported by numerous clinical trials | Limited, mostly from related conditions |
| Common Side Effects | Skin thinning, irritation, potential systemic absorption | Mild local reactions; systemic effects rare |
| Usage | Varied dosages, often daily or as prescribed | Typically once daily topical application |
In practice, ivermectin should not be viewed as a replacement but rather an adjunctive option-particularly for individuals who have eczema complicated by microbial factors or who do not respond fully to traditional therapies. Patients considering ivermectin should discuss with their dermatologist whether their eczema subtype might benefit from this approach, and consider it alongside moisturizers and established anti-inflammatory medications. Continuous monitoring and professional guidance remain critical to ensure safety and optimal outcomes.
Ultimately, while traditional eczema treatments remain the cornerstone of care with proven efficacy and safety, ivermectin offers a promising supplement for specific cases. Keeping abreast of emerging research and individualizing treatment plans offers the best path forward for achieving skin relief and improved quality of life.
Applying Ivermectin: Dosage and Administration Guidelines
Many patients find that understanding how to properly use ivermectin can enhance their eczema care, especially when traditional treatments only partly relieve symptoms. While ivermectin is not yet a standard eczema treatment, its topical form-commonly a 1% cream-has been explored for its potential to reduce inflammation and target microscopic skin mites, factors that sometimes complicate eczema. Applying it correctly ensures maximum benefit while minimizing irritation.
For those prescribed topical ivermectin, once-daily application is typically recommended. You should apply a thin, even layer to the affected areas after cleansing and drying your skin gently. Avoid applying near the eyes, mouth, or open wounds unless directed by your healthcare provider. Usually, only a small pea-sized amount is needed for each localized patch of eczema. Consistency is key-daily use over several weeks may be necessary to see results, but treatment duration should be guided by your dermatologist based on your response and skin sensitivity.
Practical Tips for Safe Application
- Cleanse gently: Use a mild, fragrance-free cleanser before applying ivermectin to reduce irritation.
- Moisturize strategically: Wait at least 20-30 minutes after applying ivermectin before using your regular moisturizer, unless advised otherwise.
- Avoid overuse: Applying more cream or using it more frequently than prescribed won’t speed healing and can increase irritation risk.
- Sun protection: Since eczema and its treatments can increase photosensitivity, use sunscreen or protective clothing if you plan to be outdoors.
Integrating Ivermectin Into Your Routine
Pairing ivermectin with established eczema management routines-like moisturizing regularly and avoiding irritants-often yields the best outcomes. For example, individuals with eczema who also have stubborn redness or itching linked to Demodex mites might see marked improvements when ivermectin is added. However, because formal dosing guidelines specific to eczema are still emerging, your dermatologist may tailor frequency or duration based on your unique skin condition and response.
| Step | Recommended Approach |
|---|---|
| Frequency | Once daily, preferably at night |
| Amount per application | Small pea-sized amount per affected area |
| Application technique | Apply a thin layer on clean, dry skin; rub in gently |
| Treatment duration | Several weeks, as advised by your dermatologist |
| Concurrent use | Moisturizers or other topical medications-apply them at different times to avoid interactions |
Always discuss your full skincare routine with your healthcare provider before starting ivermectin to avoid unintended interactions or sensitivities. If irritation or excessive dryness occurs, pause treatment and consult your dermatologist for alternatives or adjustments. Ultimately, careful application and professional guidance are vital for turning ivermectin into a valuable component of eczema care.
Potential Side Effects: What to Expect
Ivermectin is generally well-tolerated when used topically, but like all treatments, it can cause side effects, especially for those with sensitive or compromised skin such as in eczema. It’s important to recognize early signs and understand how to respond so you can continue your skincare journey safely and effectively.
Mild irritation is the most common reaction. This can include redness, slight burning, or itching shortly after application. These symptoms often subside as your skin adjusts to the medication. However, if irritation worsens or persists beyond a few days, it may indicate heightened sensitivity or an allergic response. In such cases, pausing the treatment and consulting your dermatologist is advisable to avoid worsening your eczema flare-ups.
Because ivermectin targets microscopic mites, some users might experience a temporary “die-off” reaction-a brief increase in redness or itching as the skin reacts to the elimination of these mites. While this can be uncomfortable, it’s usually a sign the medication is working. Keeping your skin well-moisturized and avoiding additional irritants during this period can help ease discomfort.
Understanding Potential Skin Reactions
- Dryness or peeling: Ivermectin can sometimes cause mild dryness. Gently moisturizing with a non-irritating product helps restore the skin barrier.
- Contact dermatitis: Though rare, some people develop allergic dermatitis to the cream’s ingredients rather than ivermectin itself.
- Photosensitivity: Ivermectin may increase skin sensitivity to sunlight, so daily use of sunscreen or protective clothing is prudent during treatment.
| Side Effect | Typical Onset | Management Tips |
|---|---|---|
| Mild irritation (redness, itching) | Days 1-7 | Reduce frequency or apply less product; use gentle moisturizers |
| Dryness or peeling | Week 1 onward | Increase hydrating skincare; avoid harsh cleansers |
| Temporary “die-off” reaction | First 1-2 weeks | Patience, moisturize, and avoid scratching |
| Allergic contact dermatitis (rare) | Variable | Discontinue, seek dermatologist advice |
Staying attentive to your body’s responses and maintaining open communication with your healthcare provider is key. Always report unusual or severe reactions promptly-this collaborative approach ensures treatment is both safe and tailored to your skin’s needs. Remember, side effects do not diminish ivermectin’s potential usefulness but highlight the importance of mindful use in the delicate context of eczema care.
Patient Experiences: Real Stories of Skin Healing
Many people with eczema report noticeable improvements after incorporating ivermectin into their treatment regimen, often describing the relief as a turning point in their skin health journey. One common theme among these experiences is the gradual reduction in inflammation and itching, which are hallmark symptoms of eczema. While initial skin reactions such as mild irritation or a “die-off” response can be unsettling, patience and proper skincare often reveal significant benefits as the treatment progresses.
- Targeting underlying triggers: Several patients note that ivermectin’s action against microscopic skin mites-factors sometimes overlooked in eczema-helps reduce persistent irritations and flare-ups that standard moisturizers and corticosteroids do not fully address.
- Improved skin texture and hydration: Over weeks of consistent use, users frequently observe softer, less cracked skin, owing to the medication’s anti-inflammatory effects combined with careful moisturizing.
- Enhanced quality of life: The relief from relentless itching leads to better sleep and reduced stress, which further benefits eczema management holistically.
Practical Advice from Users
Patients emphasize the importance of starting with a patch test to monitor sensitivity, especially for those with highly reactive skin. Many find that combining ivermectin with gentle, fragrance-free moisturizers supports better tolerance and skin repair. Avoiding aggressive scrubs or harsh soaps during treatment minimizes further irritation. Additionally, documenting skin changes, either through photos or notes, helps track progress and guide conversations with healthcare providers.
Balancing Expectations
It is worth noting that not everyone experiences dramatic improvements, and some may encounter mild side effects initially. Importantly, ivermectin is not a cure-all but a potentially valuable component of a comprehensive eczema care strategy. Patients should continue regular consultations with their dermatologists to adjust treatment plans based on their individual responses. Real success stories highlight the value of open communication and personalized care rather than quick fixes or one-size-fits-all solutions.
Ultimately, these firsthand accounts underscore ivermectin’s promise as an adjunct therapy, offering renewed hope for those struggling with stubborn eczema symptoms while reminding users to prioritize safety and professional guidance throughout their treatment journey.
Expert Opinions: Dermatologists Weigh In
Ivermectin has sparked considerable interest in dermatology due to its well-documented anti-inflammatory and antiparasitic properties. While its use for eczema remains off-label and under active research, many dermatologists acknowledge its potential as an adjunct treatment for certain patients-especially those whose eczema involves factors beyond just immune dysregulation, such as microscopic skin infestations. Experts emphasize that eczema, being a complex condition with multiple triggers, requires a personalized treatment approach rather than a one-size-fits-all solution.
Many specialists highlight ivermectin’s ability to reduce inflammatory responses and target skin mites that might contribute to persistent irritation and flare-ups. This dual action distinguishes ivermectin from traditional therapies like corticosteroids, which primarily suppress inflammation but do not address possible parasitic triggers. However, dermatologists caution against expecting ivermectin to be a standalone cure. Instead, they recommend it as part of a wider management plan that includes moisturization, avoidance of irritants, and regular medical supervision.
- Clinical prudence: Dermatologists strongly advise conducting patch tests before starting ivermectin to monitor any potential sensitivity, especially since eczema-prone skin can be highly reactive.
- Balanced expectations: Many clinicians note that while some patients report significant symptom relief-reduced itching, redness, and improved texture-others may see minimal impact. The heterogeneity of eczema means response rates vary widely.
- Integration strategy: Experts often recommend combining ivermectin with gentle skincare routines, including fragrance-free moisturizers and avoiding harsh soaps, to optimize outcomes and reduce irritation risks.
Additionally, some dermatologists underscore the importance of ongoing research to clarify ivermectin’s exact role and safety profile in eczema care. While initial data and patient reports are promising, robust clinical trials remain limited. Practitioners encourage open dialogue with patients about the current evidence, setting realistic goals and emphasizing that professional guidance and monitoring are essential for safe, effective treatment.
Ultimately, leading voices in dermatology recognize ivermectin’s promise but remind patients to remain informed and cautious. Personalized medical advice remains paramount: eczema management should be a collaborative journey tailored to individual skin needs and responses, where ivermectin might serve as a valuable tool-not a magic bullet-in the quest for healthier skin.
The Future of Eczema Treatment: Beyond Ivermectin
Eczema treatment is on the cusp of exciting advancements that go well beyond current options like ivermectin. While ivermectin offers distinct benefits by targeting both inflammation and potential parasitic contributors, researchers and clinicians are increasingly exploring innovative therapies to address the complex underlying causes of eczema. This future points toward more personalized, targeted strategies that not only calm flare-ups but may also improve long-term skin health and barrier function.
One promising frontier involves harnessing the skin’s natural microbiome-the community of beneficial bacteria living on healthy skin. Recent research reveals that certain bacterial strains can help restore balance to eczema-prone skin by inhibiting harmful microbes and reducing inflammation. Clinical trials are underway using topical probiotics designed to introduce these “good” bacteria as a therapeutic agent. These approaches represent a shift from simply suppressing symptoms to actively promoting skin resilience and healing through tailored microbial management.
Emerging Therapies in Focus
- Biologic medications: These drugs target specific molecules in the immune system responsible for eczema’s inflammatory response. Already approved biologics like dupilumab have shown significant benefits and ongoing research is expanding this class of treatments.
- Janus kinase (JAK) inhibitors: Topical and oral agents in this category interfere with key signaling pathways in skin inflammation, offering new options especially for moderate to severe eczema cases not well-controlled by traditional therapies.
- Microbiome-based treatments: Building on discoveries around skin bacteria, experimental applications like the use of _Roseomonas mucosa_ show potential to rebuild a healthier skin environment.
Personalized Approaches Will Take Center Stage
The future of eczema care will likely focus heavily on personalized regimens that consider each patient’s unique triggers, skin type, and immune responses. Combining novel therapies like microbiome restoration or biologics with lifestyle modifications-such as avoiding irritants, consistent moisturization, and stress management-can create a comprehensive, multi-layered defense against flare-ups.
For patients and caregivers, staying informed about emerging treatments through consultation with dermatologists is crucial. While the evolving landscape offers hope, medical supervision ensures that new options are used safely and effectively. Keeping realistic expectations about the timing, risks, and benefits of emerging therapies supports better long-term outcomes.
Ultimately, the landscape beyond ivermectin looks hopeful, with a growing toolbox designed to address eczema’s many dimensions. Empowered by science and personalized care, sufferers can anticipate treatments that do more than soothe symptoms-they aim to transform skin health from the inside out.
Frequently Asked Questions About Ivermectin and Eczema
Many people are surprised to learn that ivermectin, initially known for its antiparasitic properties, is gaining attention in dermatology for potential roles beyond scabies and rosacea. While eczema (atopic dermatitis) is primarily an inflammatory skin condition not caused by parasites, ivermectin’s anti-inflammatory effects and ability to target skin mites like *Demodex* have prompted curiosity about its usefulness in eczema management. However, it’s important to understand what current science says and what it does not.
Common Questions About Ivermectin Use for Eczema
- Is ivermectin an approved treatment for eczema?
As of now, ivermectin is not officially approved for treating eczema. Its primary dermatological uses are for scabies, rosacea, and other conditions involving parasites or mites. Research is ongoing, but solid clinical trial evidence for eczema specifically is limited.
What this means: Ivermectin might be prescribed off-label by some dermatologists, especially if secondary issues like *Demodex* overgrowth are suspected, but it should not replace standard eczema treatments. - How does ivermectin work in skin conditions?
Ivermectin paralyzes certain tiny mites or parasites by interfering with their nervous system. It also exhibits anti-inflammatory effects, which can help soothe redness and irritation. These dual actions make it valuable for conditions like rosacea and scabies and theoretically suggest potential benefits in eczema if microbes or inflammation are involved.
- Can ivermectin help if I have eczema with frequent itching and flare-ups?
While ivermectin may reduce inflammation, eczema’s causes are multifactorial, involving immune responses, genetics, and skin barrier dysfunction. It is unlikely to fully control eczema alone but might help in select cases-particularly where infections or mites exacerbate symptoms. Ongoing management with moisturizers, trigger avoidance, and anti-inflammatory agents remains the cornerstone.
- What forms and dosages of ivermectin are used for skin problems?
Ivermectin is available as a topical cream (typically 1%) and oral tablets. For skin infestations, topical application is common. Oral ivermectin is sometimes used for widespread infestations like scabies, dosed by body weight (for example, 200-400 μg/kg). Consult a healthcare provider for appropriate dosing and regimen based on individual needs.
- Are there side effects to be aware of?
Side effects of topical ivermectin are usually mild and may include skin irritation or dryness. Oral ivermectin can cause headache, dizziness, or gastrointestinal symptoms in some cases. Serious side effects are rare but possible. Always discuss risks versus benefits with a dermatologist before starting treatment.
Practical Tips When Considering Ivermectin for Eczema
- Consult a dermatologist: Never self-medicate with ivermectin. Expert guidance ensures correct diagnosis and safe use.
- Use as part of a broader plan: Ivermectin is not a cure-all. Combine it with proven eczema treatments like moisturizers and prescribed anti-inflammatories.
- Monitor your skin closely: Track improvements or side effects so your healthcare provider can adjust therapy if needed.
- Report any unusual symptoms immediately: This includes severe itching, rash, or any systemic effects.
Understanding that ivermectin’s role in eczema is still emerging prevents unrealistic expectations while appreciating its promise as part of evolving skin care strategies. Keeping an open dialogue with your healthcare team allows safe, informed decisions as new research unfolds.
| FAQ | Key Points |
|---|---|
| Is ivermectin approved for eczema? | Not officially; used mainly off-label with dermatologist guidance |
| How does it work? | Targets mites & parasites; reduces inflammation |
| Forms and doses? | Topical 1% cream; oral tablets at weight-based doses |
| Common side effects? | Mild skin irritation (topical); headache, dizziness (oral) |
| Should I self-treat? | No, always seek professional advice |
Lifestyle Tips for Managing Eczema Alongside Treatment
Many people underestimate the power of daily habits in managing eczema effectively alongside medical treatments. Small lifestyle adjustments can significantly reduce flare-ups, improve skin barrier function, and support the healing process when using therapies like ivermectin. Recognizing eczema as a multifactorial condition involving immune response, skin dryness, and environmental triggers helps highlight why an integrated approach is vital for long-term relief.
Create a Skin-Friendly Environment
Maintaining optimal humidity and cleanliness can make a noticeable difference. Dry air can worsen eczema by stripping natural skin moisture, so using a humidifier during colder months or in dry climates helps keep the skin hydrated. Additionally, minimizing exposure to harsh soaps, detergents, and synthetic fragrances reduces irritants that often provoke eczema flare-ups. Opt for mild, fragrance-free cleansers and laundry products designed for sensitive skin.
Master the Art of Gentle Skin Care
Regular moisturizing with emollients supports the skin’s natural barrier, reducing itching and irritation. Applying moisturizers immediately after bathing helps lock in moisture. Choose creams or ointments over lotions, as these types better seal moisture. When considering ivermectin or other topical therapies, apply them only on clean, dry skin and follow your healthcare provider’s specific guidelines to avoid compounding irritation. Avoid hot showers and vigorous scrubbing, which can aggravate vulnerable skin.
Identify and Manage Personal Triggers
Eczema triggers vary widely-from stress and allergens to sweat and certain fabrics. Keeping a symptom diary can help uncover patterns and inform personalized avoidance strategies. For instance, some people find wool or synthetic clothing irritating, while others react to pollen or pet dander. Stress management techniques such as mindfulness, yoga, or gentle exercise may also reduce flare frequency by calming inflammatory responses linked to eczema.
Nutrition and Hydration Matter Too
While diet alone does not cure eczema, staying well-hydrated supports skin health, and some studies suggest that balanced nutrition rich in antioxidants and omega-3 fatty acids can modulate inflammation. Including foods like fatty fish, nuts, and colorful fruits and vegetables may offer mild benefits. Always discuss any dietary changes with your healthcare provider to ensure they complement your eczema management plan.
- Consult regularly with your dermatologist: Your provider can adjust treatments like ivermectin based on your skin’s response and evolving needs.
- Avoid self-treatment jumps: Combining lifestyle changes with professional advice enhances safety and effectiveness.
Adopting these practical strategies, alongside any prescribed treatment, empowers you to take control of eczema symptoms and support your skin’s healing journey with confidence.
Faq
Q: Can Ivermectin help with eczema flare-ups triggered by skin infections?
A: Yes, Ivermectin’s anti-parasitic and anti-inflammatory properties can reduce eczema flare-ups linked to skin infections like mites or bacteria. It targets skin-dwelling parasites that may worsen eczema symptoms, providing relief and promoting clearer skin. Always consult a dermatologist before use for best results.
Q: How does Ivermectin compare to corticosteroids for eczema treatment?
A: Ivermectin offers a non-steroidal alternative by targeting inflammation and parasites without the risk of skin thinning associated with corticosteroids. It may be preferable for long-term eczema management, especially in sensitive areas. Discuss with your doctor to determine the best treatment approach for your skin.
Q: Is topical Ivermectin safe to use on sensitive or broken eczema skin?
A: Topical Ivermectin is generally safe but should be used cautiously on sensitive or broken eczema skin to avoid irritation. Patch testing and medical guidance are recommended to minimize side effects, ensuring safe integration into your skincare routine.
Q: Can Ivermectin be combined with moisturizers and other eczema treatments?
A: Yes, Ivermectin can be safely combined with moisturizers and other eczema therapies like emollients or antihistamines. Combining treatments supports skin hydration and symptom relief but always follow your healthcare provider’s advice to avoid interactions.
Q: How long does it take to see improvement in eczema symptoms after starting Ivermectin?
A: Improvement with Ivermectin typically appears within 2 to 4 weeks of consistent use. Patients often notice reduced redness and itching as inflammation decreases. For best outcomes, follow dosage guidelines detailed in the article’s application section.
Q: Are there any specific skin types that respond better to Ivermectin for eczema?
A: Ivermectin may be particularly effective for eczema associated with parasitic involvement or severe inflammation, regardless of skin type. However, those with dry or sensitive skin should monitor for irritation and consult a dermatologist to tailor treatment.
Q: What lifestyle changes enhance Ivermectin’s effectiveness in eczema healing?
A: Maintaining consistent skin moisturizing, avoiding known eczema triggers, and gentle cleansing routines enhance Ivermectin’s anti-inflammatory benefits. These lifestyle tips, covered in the article’s management section, support skin barrier repair and faster healing.
Q: Can I use Ivermectin preventatively to reduce eczema outbreaks?
A: Preventative use of Ivermectin may help reduce eczema outbreaks caused by skin parasites or inflammation, but it is best used under medical supervision. Consult your healthcare provider to develop a safe, personalized prevention plan aligned with your eczema triggers.
Feel free to explore the full article for detailed guidance on Ivermectin application, patient experiences, and expert advice to empower your eczema treatment journey.
Closing Remarks
Discovering ivermectin’s potential in easing eczema symptoms opens new doors for skin healing. While it’s not a universal remedy, this breakthrough highlights an innovative path worth exploring. If you’re curious about how ivermectin or alternative treatments might fit your skin health routine, now is the time to learn more and consult your healthcare provider for personalized advice.
Ready to dive deeper? Explore our detailed resources on eczema management, skin barrier repair, and emerging therapies. Signing up for our newsletter ensures you stay updated on the latest scientific insights and practical tips. Share your experiences or questions below-your engagement helps us build a supportive community focused on skin wellness.
By revisiting this topic and related areas like anti-inflammatory treatments and dermatological research, you increase your knowledge and empower yourself with options. Together, let’s navigate eczema care with confidence, backed by science and genuine support.






