Did you know scabies mites can live on your skin for months, causing intense itching and discomfort? Finding an effective treatment is essential to stop the spread and ease symptoms. Ivermectin, a prescription antiparasitic medication, has gained recognition for its success in treating scabies, especially in cases where topical treatments may be less practical. This oral medication works by targeting the mites systemically, offering a convenient option backed by science and global health authorities. If you or someone you know is struggling with scabies, learning about real-world experiences with ivermectin can provide valuable insights and hope. While ivermectin shows promising results, it’s important to approach treatment under medical supervision, as correct usage and simultaneous treatment of close contacts are key to full recovery. In this article, we’ll explore proven success stories and what makes ivermectin a trusted choice in managing this contagious skin condition, helping you make informed decisions on your health journey.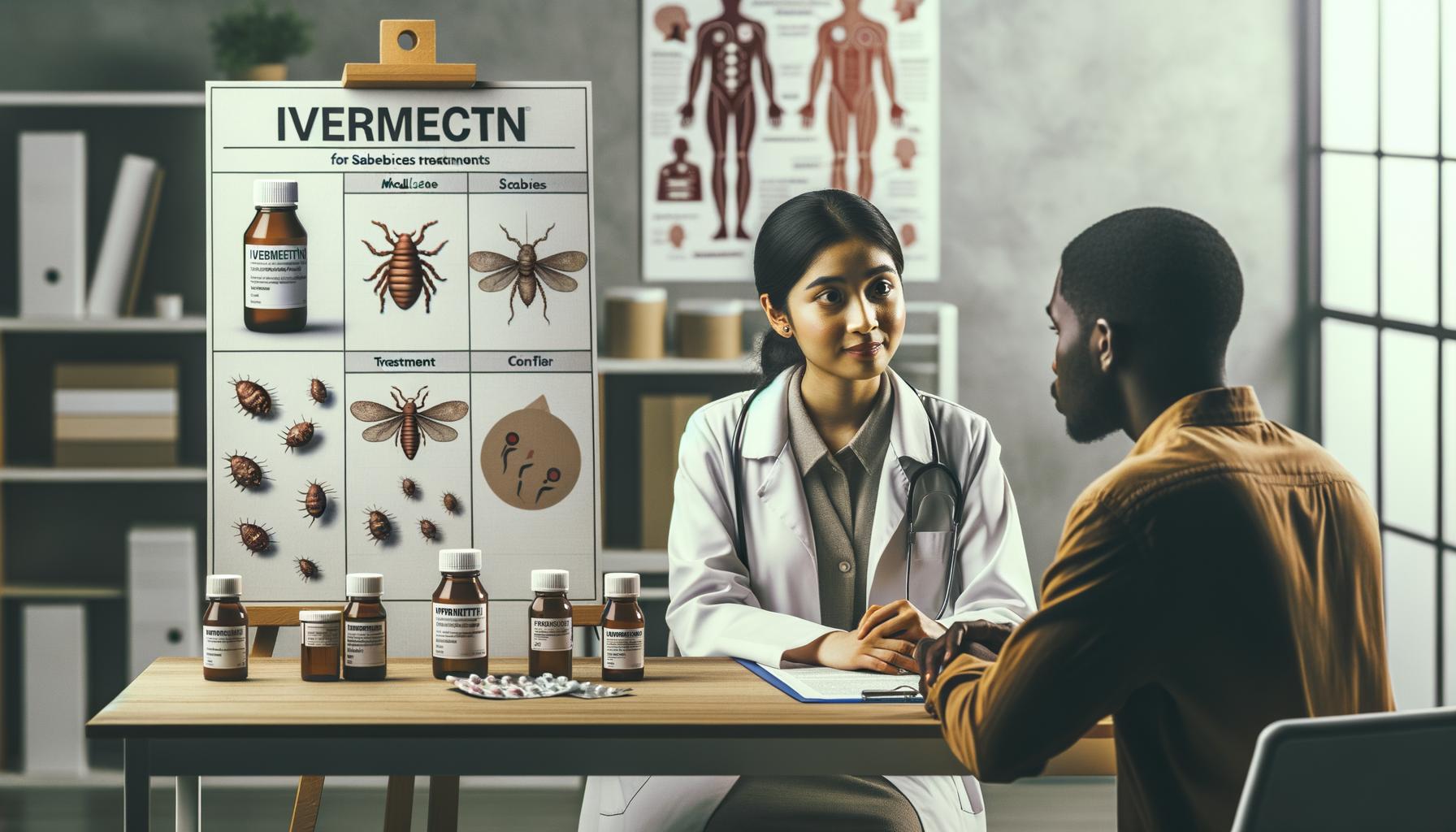
Ivermectin: What You Need to Know for Scabies
Ivermectin has transformed scabies treatment for many people, particularly in cases where traditional topical creams may fall short. As an oral medication, it provides a convenient and effective alternative that targets the mites responsible for scabies from within the body. This is especially beneficial for individuals with crusted (severe) scabies or those who have weakened immune systems, where topical treatments alone might not be sufficient.
What Makes Ivermectin a Valuable Option?
Ivermectin works by interfering with the nerve and muscle functions of the scabies mites, effectively paralyzing and killing them. Because it is taken orally, it reaches areas of the skin that might be missed with creams or lotions. This can lead to a faster reduction in symptoms such as intense itching and rash. However, it’s important to remember that ivermectin is usually prescribed when initial topical treatments do not work or are unsuitable.
Important Considerations Before Use
While ivermectin is generally well tolerated, it is not recommended for everyone. Pregnant or nursing women and children weighing less than 33 pounds (15 kilograms) are typically advised to avoid this medication due to potential risks. Always consult a healthcare provider to ensure it’s safe based on your personal health history. Additionally, ivermectin treatment often involves one or two doses spaced a week apart to maximize effectiveness and ensure complete eradication of mites.
Practical Tips for Patients
- Follow the dosing schedule exactly: Skipping doses or taking too much will reduce effectiveness and may increase side effects.
- Complement treatment with skin care: Use soothing agents or antihistamines to manage itching while the medication works.
- Be patient with symptom relief: Itching can persist for a week or two even after mites are eliminated as the skin heals.
Choosing ivermectin can be a practical step in resolving stubborn or widespread scabies infections. Its convenience and systemic action make it a crucial tool, but balanced with awareness of its limitations and potential side effects. Always partner with your healthcare provider for the best outcome and to tailor treatment to your unique needs.[[1]][[2]]
Understanding Scabies: Symptoms and Diagnosis
Scabies is a highly contagious skin condition caused by tiny mites that burrow into the upper layer of the skin. One of the most distinctive and troubling features is intense itching, especially at night, which often disturbs sleep and daily comfort. The rash caused by scabies can appear as small bumps, blisters, or lines where the mites tunnel beneath the skin, commonly found between fingers, on the wrists, elbows, or around the waist. Understanding these symptoms early is key to seeking timely treatment and reducing transmission.
Accurate diagnosis often requires a healthcare provider to closely examine the skin. They may look for characteristic burrows or lesions and consider your history of close contact with others who might be infected. Sometimes, a skin scraping under a microscope is needed to identify the mites, eggs, or fecal matter, though this is not always necessary. Because symptoms can resemble other skin conditions such as eczema or allergic reactions, professional evaluation is important to avoid misdiagnosis.
- Common symptoms: Intense itching (especially at night), pimple-like irritations, and burrow marks.
- Typical locations: Between fingers, wrists, elbows, waistline, and genital areas.
- Transmission clues: Close physical contact with an infected person or sharing bedding and clothing.
It’s worth noting that symptoms may take several weeks to appear after initial exposure, which can delay diagnosis. Additionally, people with repeated or severe scabies infections might show more widespread symptoms, including thick crusts on the skin, making detection more challenging.
Consulting a healthcare professional is essential when scabies is suspected, as early diagnosis allows for effective treatment plans such as ivermectin or topical therapies. Delaying care increases discomfort and the risk of spreading mites to others. Remember, scabies is manageable with a careful approach, and understanding the symptoms and diagnosis process empowers you to act decisively and confidently to reclaim your skin health.[[2]][[1]]
The Science Behind Ivermectin as a Treatment
Ivermectin works by targeting the nervous system of the scabies mite, effectively paralyzing and killing these microscopic parasites. Unlike topical treatments that need direct contact with the affected skin, oral ivermectin enters the bloodstream and reaches mites hidden beneath the skin’s surface. This systemic action makes it especially useful for treating tough cases such as crusted scabies or widespread infestations where topical treatments might be less practical.
How Ivermectin Disrupts Mite Function
Ivermectin binds to specific nerve and muscle cell receptors in the mites, known as glutamate-gated chloride channels. This causes an influx of chloride ions, leading to hyperpolarization and paralysis of the parasite. Without the ability to move or feed, the mites die naturally and are then cleared by the body’s immune system. Humans lack these receptors, which is why ivermectin can be selective for mites without harming the patient when used properly.
Advantages of Oral Ivermectin
- Systemic Reach: It treats mites located deep under the skin or in hard-to-reach areas.
- Convenience: Oral dosing is easier for large-scale outbreaks or patients who struggle with topical applications.
- Effectiveness: Clinical studies show that oral ivermectin has comparable cure rates to topical permethrin, especially when two doses are given 7 to 14 days apart.[[2]]
It’s important to note that ivermectin does not kill mite eggs, so multiple doses are typically needed to interrupt the life cycle. Additionally, ivermectin is often combined with topical treatments for enhanced efficacy in resistant or severe cases. Because it’s not FDA-approved specifically for scabies, using ivermectin should always involve consultation with a healthcare professional to determine appropriate dosing and follow-up.
Understanding the science behind ivermectin clarifies why it has become a valuable tool against scabies, offering hope to those dealing with persistent or complicated infestations. Its mechanism of action exploits the mites’ vulnerabilities while being well-tolerated in humans, balancing safety with strong clinical effectiveness.[[1]] [[3]]
Proven Success Stories: Real-Life Ivermectin Experiences
Many people battling scabies have found relief through ivermectin, especially those facing severe or stubborn infestations. Unlike topical treatments that require precise application, ivermectin’s oral form offers a systemic approach that often leads to faster and more thorough eradication of mites, even in hard-to-treat cases. Patients frequently share how two doses of oral ivermectin, spaced a week or two apart, have dramatically reduced itching and rash, allowing them to return to normal daily life.
One common experience involves individuals who struggled with intense itching and sleepless nights for weeks before trying ivermectin. After consulting healthcare providers and receiving the medication, they report significant improvements within days, not only from the physical symptoms but also from the emotional distress that scabies can cause. This quick response helps break the cycle of reinfestation by reducing scratching, which otherwise damages skin and increases infection risk.
What Patients Want You to Know
- Follow-Up Is Crucial: Many remind that since ivermectin doesn’t kill mite eggs, a second dose is vital to complete treatment and prevent relapse.
- Combine With Skin Care: Using soothing topical therapies or antihistamines alongside ivermectin can ease itching and speed healing.
- Consult Professionals: Because scabies diagnosis can be tricky, proper medical evaluation ensures ivermectin is appropriate and dosing is correct.
In community outbreaks or crusted scabies cases, ivermectin has been a game changer. Clinics report success in controlling infestations where topical treatments alone failed or were impractical due to widespread skin involvement. While responses vary, shared stories consistently highlight benefits like convenience, tolerability, and effectiveness, giving many a second chance to regain comfort and confidence.
Ultimately, these real-world experiences reinforce ivermectin’s value as part of the scabies treatment toolkit. Patients considering it should engage healthcare providers to tailor therapy to their needs, ensuring the best possible outcome based on their unique situation.
How to Use Ivermectin for Scabies Effectively
Ivermectin’s effectiveness in treating scabies relies heavily on following a carefully timed dosing schedule. Typically, treatment involves two oral doses spaced one to two weeks apart. This gap is crucial because ivermectin targets the live mites but does not reliably kill their eggs. The second dose helps eliminate newly hatched mites before they can mature and continue the infestation. Missing this second dose or incorrect timing can lead to treatment failure or recurrence.
Taking ivermectin with food can enhance absorption and improve results, so it’s advisable to eat a light meal beforehand. It’s equally important to complete the full prescribed course even if symptoms start to improve quickly. Many patients report significant relief within days of the first dose, but the residual itch and rash can linger for a while as the skin heals. Combining ivermectin with supportive skin care, such as soothing creams or oral antihistamines, can ease discomfort during this recovery phase.
Key Practices for Maximizing Ivermectin’s Impact
- Treat Close Contacts Simultaneously: Scabies spreads easily through skin-to-skin contact. All household members and close contacts should receive treatment at the same time-even if they show no symptoms-to prevent reinfestation.
- Maintain Good Hygiene and Environment Care: Wash bedding, clothing, and towels in hot water and dry on high heat. Non-washable items can be sealed in plastic bags for several days to starve mites.
- Consult Your Healthcare Provider: Since dosing may vary based on weight, age, and severity, always follow medical advice. Some patients with crusted scabies or widespread disease may require multiple doses or combination therapy with topical agents.
By approaching ivermectin treatment thoughtfully-respecting the timing, supporting skin healing, and addressing environmental factors-patients can significantly improve their chances of a swift, lasting recovery. Real-world experiences consistently highlight that adherence to these steps empowers people to regain comfort and confidence, often after months of persistent symptoms. Remember, ongoing communication with your healthcare provider ensures adjustments can be made as needed for your unique situation [[1]](https://cdn.bad.org.uk/uploads/2023/10/Scabies-guidance-OCT-2023.pdf) [[2]](https://pmc.ncbi.nlm.nih.gov/articles/PMC6494415/) [[3]](https://www.rivm.nl/en/scabies/treating-scabies/ivermectin-tablets).
Potential Side Effects and Precautions
Ivermectin is generally well tolerated, but like any medication, it carries the potential for side effects that users should be aware of. Understanding these possible reactions helps you make informed decisions and recognize when to seek medical advice during scabies treatment. Many individuals experience mild side effects that resolve quickly, while serious reactions remain uncommon.
Most commonly, patients report symptoms such as dizziness, mild nausea, or headache shortly after taking ivermectin. Some may notice fatigue or temporary shaking. These effects tend to be transient and do not require stopping treatment. Skin-related reactions-such as itching, rash, or swelling-can also occur, often reflecting the body’s response to dying mites rather than a direct drug allergy. This “post-treatment itch” sometimes leads to confusion but usually improves with soothing skincare or antihistamines as part of supportive care.
Key Precautions to Keep in Mind
- Medical History Matters: People with liver problems, weakened immune systems, or neurological conditions should inform their healthcare provider before starting ivermectin, as dose adjustments or alternative therapies might be necessary.
- Avoid Self-Medication or Unverified Sources: Ivermectin obtained outside prescribed guidance or intended for other uses (like veterinary formulations) poses significant risks and should be strictly avoided.
- Drug Interactions: Discuss any other medications or supplements you take with your doctor, since ivermectin can interact, albeit rarely, with some drugs, potentially affecting safety or effectiveness.
- Pregnancy and Children: Ivermectin’s safety profile in pregnancy or young children varies; always seek professional advice before use in these populations.
| Side Effect | Frequency | Management Tips |
|---|---|---|
| Dizziness | Common | Rest, avoid driving until resolved |
| Mild nausea | Common | Take with food and stay hydrated |
| Itching or rash | Common | Use soothing creams, antihistamines |
| Swelling (rare allergic reaction) | Rare | Seek immediate medical attention |
Real-world experiences emphasize the importance of following prescribed dosing and timing carefully to minimize both side effects and treatment failures. For instance, some patients have found that taking ivermectin with a light meal reduces nausea, while others benefited from preemptive skin care measures to soothe the temporary irritation caused by mite die-off. Open dialogue with your healthcare provider ensures that any side effects are promptly addressed and that adjustments can be made if discomfort persists.
Remember, the benefits of ivermectin in effectively clearing scabies generally outweigh the risks when used responsibly under medical supervision. If unusual or severe symptoms occur, immediate consultation is vital. Empowered with knowledge about side effects and safety measures, you can approach treatment confidently while safeguarding your health [[1]](https://www.medicinenet.com/ivermectin/article.htm) [[2]](https://www.webmd.com/drugs/2/drug-1122/ivermectin-oral/details) [[3]](https://www.drugs.com/sfx/ivermectin-side-effects.html).
Comparing Ivermectin to Other Scabies Treatments
Ivermectin stands out in the scabies treatment landscape primarily for its convenience and systemic action, which differs notably from traditional topical options. Unlike creams or lotions that must be applied to the entire body surface, ivermectin is taken orally, making it easier to use-especially for those who find topical application cumbersome or uncomfortable. This systemic approach also targets mites hidden deep within the skin layers, which topical treatments might miss.
However, topical agents like permethrin cream remain a first-line treatment in many cases due to their localized effect and well-established safety profile. Permethrin requires careful and thorough application to all affected areas and sometimes repeated treatments. Some patients find its application time-consuming but appreciate the minimal systemic absorption, reducing concerns about broader side effects.
Comparing Effectiveness and Convenience
- Ivermectin: Oral dosing typically involves one or two pills spaced a week apart. It’s especially useful in crusted scabies or outbreaks in institutions where treating many people quickly is necessary.
- Permethrin and Other Topicals: These require direct skin application, usually overnight. They effectively eradicate mites but depend heavily on proper application technique to avoid treatment failure.
- Combination Approaches: Some studies suggest that combining ivermectin with topical treatments can improve clearance rates, particularly in resistant or severe cases.
Real-world reports reveal patients appreciate ivermectin for its simplicity but often pair it with topical treatments to soothe itching and support skin healing. Importantly, no treatment is universally perfect-choice depends on individual preferences, severity of infestation, and underlying health. Consulting a healthcare provider ensures that the selected treatment matches personal needs and circumstances.
| Treatment | Mode of Use | Pros | Cons |
|---|---|---|---|
| Ivermectin | Oral pill | Easy dosing, systemic reach, good for severe cases | Possible mild side effects, not suitable for all populations |
| Permethrin Cream | Topical application | Local effect, minimal systemic absorption | Requires thorough application, can cause skin irritation |
| Benzyl Benzoate | Topical lotion | Effective in resource-limited settings | Stronger irritation, unpleasant odor |
In summary, while ivermectin offers a practical, effective alternative to traditional topical therapies, the best scabies treatment plan balances ease of use, patient tolerance, and clinical efficacy. Always seek guidance from a healthcare professional to determine which option suits your situation best and to ensure safe, effective treatment [[1]](https://www.drugs.com/dosage/ivermectin.html) [[2]](https://pmc.ncbi.nlm.nih.gov/articles/PMC6494415/) [[3]](https://www.verywellhealth.com/scabies-home-remedies-5221860).
What to Expect During Treatment with Ivermectin
One of the most reassuring facts about ivermectin treatment for scabies is how straightforward the process tends to be. After taking the oral dose-typically a single pill or sometimes a follow-up dose after 7 to 14 days-many patients notice improvement within a week. However, it’s important to understand that even as the medication kills the mites, residual itching and skin irritation can persist for several weeks. This happens because the body continues to react to mite debris and eggs, which can trigger an inflammatory response even after the parasites themselves are eliminated.
What You Might Experience
- Initial Relief and Persistent Itching: You may feel some symptom relief within a few days, but itching often continues despite the mites being killed. This is normal and does not necessarily mean the treatment failed.
- Skin Healing Takes Time: Red bumps, sores, or crusts where mites lived will slowly fade, but the skin can remain sensitive. Using gentle moisturizing creams and avoiding harsh soaps can aid recovery.
- Follow-Up Dosing: Many treatment plans include a second ivermectin dose about a week after the first to catch any newly hatched mites. Missing this second dose may reduce the chance of complete clearance.
- Consultation and Monitoring: Keep in touch with your healthcare provider if symptoms persist beyond 4 weeks or worsen, as retreatment or additional topical therapies might be needed.
Managing Expectations and Support
For some, the journey through scabies treatment with ivermectin can feel slow because itching can flare temporarily after the medication starts working. This phenomenon is called a post-scabietic itch and is a sign your immune system is clearing the remnants of the infestation. Supportive care-such as antihistamines or mild corticosteroid creams prescribed by your doctor-can make this phase more tolerable.
Patients with crusted scabies or weakened immune systems may require more prolonged treatment cycles and closer follow-up, but many find ivermectin pivotal in managing tough cases effectively. For example, individuals in nursing homes or large households appreciate the convenience of oral treatment combined with environmental measures to prevent reinfestation.
| Key Points During Ivermectin Treatment | Tips for a Smoother Experience |
|---|---|
| Possible continued itching even after mites are killed | Use gentle skin care, moisturizers, and avoid irritants |
| Follow-up dose usually needed after 7-14 days | Mark your calendar and adhere strictly to treatment schedule |
| Residual skin lesions take weeks to resolve | Be patient and protect skin from scratching |
| Consult healthcare provider if symptoms worsen or persist beyond a month | Promptly seek professional advice for possible retreatment |
Overall, understanding these treatment dynamics helps patients stay empowered and reduces frustration. Remember, clearing scabies takes more than just killing mites-it requires patience, cover of follow-up doses, and supportive skin care. Always follow your doctor’s instructions closely and contact them promptly if concerns arise, ensuring the best chance at a full, comfortable recovery[[1]](https://www.mayoclinic.org/diseases-conditions/scabies/diagnosis-treatment/drc-20377383) [[3]](https://nextstepsinderm.com/derm-topics/oral-ivermectin-therapeutic-cheat-sheet/).
Tips for Preventing Scabies Recurrences
Scabies mites are highly contagious and can easily spread through close contact or shared items, making reinfestation a common concern even after successful treatment. To minimize the risk of recurrence, it’s crucial to approach prevention from multiple angles-personal, environmental, and social.
First, maintaining rigorous hygiene practices helps limit mite transmission. This includes washing bedding, clothing, and towels in hot water and drying them on high heat to kill any surviving mites or eggs. Items that cannot be washed can be sealed in plastic bags for at least 72 hours, as mites typically cannot survive longer without human contact. Regular cleaning of frequently touched surfaces and avoiding sharing personal items like clothing or bedding are equally important measures.
Personal and Household Precautions
- Treat Close Contacts Simultaneously: Because scabies easily spreads among household members or close contacts, treating everyone at the same time-regardless of symptoms-helps break the cycle of reinfestation.
- Follow Complete Treatment Courses: Strict adherence to ivermectin dosing schedules is vital. Missing doses or skipping follow-up treatments increases the chance that some mites survive and cause a relapse.
- Avoid Skin-to-Skin Contact: During and shortly after treatment, reducing prolonged skin contact with others can help prevent passing mites back and forth.
Beyond direct contact prevention, understanding that scabies can persist in communal living environments is key. Places like nursing homes, dormitories, or crowded households require coordinated efforts-including environmental cleaning and monitoring-to keep scabies at bay. One real-world example comes from a patient living in a multi-family home who found success only after all residents underwent concurrent treatment and thorough cleaning of shared spaces, highlighting that prevention isn’t just individual but collective.
Ongoing Vigilance Supports Long-Term Success
Remaining aware of early symptoms and communicating promptly with your healthcare provider if itching or skin changes reappear also helps catch possible recurrences before they escalate. Some patients benefit from periodic check-ups especially in settings where exposure risk is higher.
| Preventive Action | Reason |
|---|---|
| Wash clothes and bedding in hot water | Kills mites and eggs on fabrics |
| Seal unwashable items in plastic for 72+ hours | Starves mites without host contact |
| Treat all close contacts at once | Prevents re-exposure within households |
| Adhere strictly to ivermectin dosing schedule | Ensures thorough mite eradication |
| Avoid sharing personal items | Reduces mite transmission risk |
By combining these strategies with clear communication and medical guidance, patients can greatly reduce the chances of scabies returning. Prevention after treatment is as essential as the therapy itself, offering a more comfortable, itch-free future and turning proven ivermectin success stories into lasting freedom from scabies infestation. Always consult your healthcare provider for tailored advice that fits your living situation and health needs[[1]](https://www.mayoclinic.org/diseases-conditions/scabies/diagnosis-treatment/drc-20377383) [[3]](https://www.verywellhealth.com/scabies-home-remedies-5221860).
Expert Insights: Dermatologists Weigh In on Ivermectin
Ivermectin has emerged as a valuable tool in treating scabies, particularly for cases where topical therapies may be challenging to apply or less effective. Dermatologists often highlight its ease of use and systemic approach, which allows ivermectin to reach mites that invade deeper layers of the skin or are missed by creams. However, experts emphasize that ivermectin is part of a broader treatment strategy, not a standalone cure. Careful diagnosis, patient education, and adherence to prescribed dosing schedules are key components that enhance its success.
Many dermatologists note that ivermectin tends to be especially helpful in managing crusted (Norwegian) scabies-a severe form where mite burdens are exceptionally high. In these situations, multiple doses spaced one to two weeks apart may be necessary to fully eradicate the infestation. Still, experts caution about its use during pregnancy or breastfeeding and advise careful benefit-risk discussions with healthcare providers. Resistance concerns also prompt clinicians to combine ivermectin with topical agents like permethrin cream for improved outcomes and reduced relapse rates[[1]](https://www.drugs.com/dosage/ivermectin.html) [[3]](https://cks.nice.org.uk/topics/scabies/prescribing-information/ivermectin/).
Practical Tips from the Clinic
- Complete the full treatment course: Dermatologists stress that skipping doses or failing to treat close contacts simultaneously can undermine ivermectin’s effectiveness.
- Monitor symptoms closely: Patients should report persistent or worsening itching after treatment, as this might indicate reinfestation, drug resistance, or secondary skin conditions.
- Combine therapies when appropriate: For stubborn or complicated cases, experts often recommend pairing ivermectin with topical treatments and environmental cleaning to ensure comprehensive mite clearance.
Real-world clinical experience reinforces that patient engagement plays a critical role. Those who understand the necessity of hygiene measures, full-course medication intake, and timely communication with their healthcare team typically see better results. Dermatologists also advise ongoing vigilance post-treatment, especially in communal living settings where reinfestation risk remains elevated.
By embracing a balanced, evidence-based approach, clinicians advocate for ivermectin as an effective component in the broader scabies management toolkit-one that can offer relief and lasting resolution when used thoughtfully and under medical supervision.
Patient Testimonials: Overcoming Scabies Challenges
Many people struggling with scabies have found renewed hope and relief after starting ivermectin treatment, sharing stories that highlight both its strengths and challenges. One common thread is the sense of regaining control over a frustrating condition that often disrupts sleep, daily activities, and overall well-being. Patients frequently describe the initial itching and discomfort as overwhelming, but after a complete medical treatment including ivermectin, many report significant improvement within days to weeks.
Real Experiences Highlight Important Lessons
Some individuals recount how combining oral ivermectin with prescribed topical creams and thorough environmental cleaning helped eliminate the infestation fully. For example, a patient with crusted scabies, which involves a heavy mite load and thicker crusted skin, explained that the multiple doses of ivermectin spaced two weeks apart, under close medical supervision, were crucial to their recovery. This underscores the critical importance of following prescribed schedules and not skipping doses to prevent treatment failure or relapse.
Others emphasize that personal vigilance after treatment is key. Persistent itching does not always indicate treatment failure; it can also be a normal part of healing or a signal of secondary skin irritation. These patients advise others to stay in close touch with their healthcare providers if symptoms persist or worsen, as adjustments or additional therapy might be needed. A few shared their experience of initial disappointment when topical therapies alone were ineffective but found swift relief after ivermectin was introduced, particularly in cases where applying creams was difficult or impractical.
Advice from Those Who’ve Been Through It
- Stick to the full treatment plan: Completing all doses as prescribed is vital to clear scabies completely.
- Treat close contacts simultaneously: Many stress that everyone in the household or close environments should be treated at the same time to avoid reinfestation.
- Maintain hygiene and environmental cleaning: Washing bedding, clothes, and cleaning living spaces extensively supports treatment success.
- Stay patient, monitor symptoms: Itching may linger after mites are gone; follow-up with your doctor if symptoms persist or worsen.
The collective insight from these personal accounts encourages patients not to lose hope, even when facing severe or persistent cases. While ivermectin is a powerful tool, success is often tied to a comprehensive approach including patient education, clear communication with healthcare providers, and an understanding of the treatment’s limitations. These stories remind readers that eradication is achievable and that medical guidance remains crucial throughout the process.
By sharing honest experiences, patients empower others to make informed choices, navigate setbacks confidently, and pursue lasting relief from scabies with a well-rounded treatment plan that includes ivermectin where appropriate[[1]](https://nextstepsinderm.com/derm-topics/oral-ivermectin-therapeutic-cheat-sheet/) [[3]](https://www.mayoclinic.org/diseases-conditions/scabies/diagnosis-treatment/drc-20377383).
FAQ
Q: How quickly can ivermectin show results in treating scabies?
A: Ivermectin typically begins reducing scabies symptoms within 1 to 2 days after the first dose, but complete clearance may take 2 to 4 weeks. Follow-up doses are important to fully eradicate mites and avoid reinfestation. Patience and adherence to dosage are key for proven treatment success.
Q: Can ivermectin be used to treat scabies outbreaks in group settings?
A: Yes, ivermectin is effective for managing scabies outbreaks in institutions like nursing homes or prisons. Mass treatment with oral ivermectin can quickly control spread when combined with hygiene measures. This approach is supported by multiple success stories in public health settings.
Q: Why do some patients need a second or third dose of ivermectin for scabies?
A: Some cases require repeat ivermectin doses due to mite resistance, reinfestation, or suboptimal initial treatment. Two doses given 7-14 days apart are standard, but additional treatments may be necessary for stubborn infections, ensuring full clearance and long-term success.
Q: Is ivermectin safe for children and pregnant women with scabies?
A: Ivermectin is generally not recommended for children under 15 kg or pregnant women without medical supervision. Safer alternatives, like topical permethrin, are preferred. Always consult a healthcare provider to determine the best and safest treatment option.
Q: How does ivermectin compare to permethrin in real-world scabies treatment outcomes?
A: Real-world studies show ivermectin and permethrin have similar cure rates when used correctly. Ivermectin’s oral form offers convenience and good efficacy, especially for widespread scabies or cases difficult to treat with creams. Choice depends on patient needs and scabies severity.
Q: What should patients do if scabies symptoms persist after ivermectin treatment?
A: Persistent symptoms may be due to mite resistance, reinfestation, or allergic reactions. Consult a healthcare professional to reassess diagnosis, possibly repeat treatment, or combine with topical therapies. Prompt action helps avoid ongoing discomfort and ensures effective recovery.
Q: Can ivermectin prevent scabies from spreading to family members?
A: Ivermectin can reduce scabies transmission by eliminating mites in treated individuals. For prevention, simultaneous treatment of close contacts and thorough cleaning of bedding and clothing are essential to avoid reinfestation and protect family health.
Q: How does food intake affect the absorption and effectiveness of oral ivermectin for scabies?
A: Taking ivermectin with food, especially a fatty meal, improves its absorption and treatment effectiveness. For optimal results, patients should follow dosing instructions carefully, including timing with meals, to maximize the drug’s success in clearing scabies.
*For further detailed insights and personal success stories with ivermectin treatment, consider reviewing the patient testimonials and expert advice sections of this article.*
Final Thoughts
Discovering how ivermectin effectively tackles scabies offers hope for lasting relief and improved skin health. This trusted treatment, backed by scientific evidence and real success stories, highlights its role in managing scabies with well-tolerated dosing regimens. Remember, early action and consultation with healthcare professionals can ensure the best outcomes, especially when considering individual factors like pregnancy or breastfeeding.
Ready to learn more about managing scabies or explore additional treatments? Dive into our comprehensive resources, expert guides, and patient experiences to empower your next steps. Don’t forget to join our newsletter for updates on skin health breakthroughs and share your thoughts or questions below-your engagement helps build a community of informed individuals overcoming scabies together.
Keep exploring related topics such as scabies symptoms, prevention strategies, and alternative therapies to deepen your understanding. By staying informed and proactive, you’re choosing a healthier future with confidence and clarity.






